What Is the Gut-Liver-Brain Axis?
The gut-liver-brain axis describes how these three organs communicate through blood flow, immune signals, and the nervous system.
Think of your liver's function as a filter sitting between your gut and the rest of your body. Your gut and liver connect through the portal vein. Everything absorbed from your intestines passes through the liver first. When the gut barrier is healthy, it filters out harmful substances. When compromised, toxins reach the liver and trigger inflammation.
The liver and brain communicate through inflammatory markers and metabolites. When liver inflammation increases, it affects mood, cognition, and sleep.
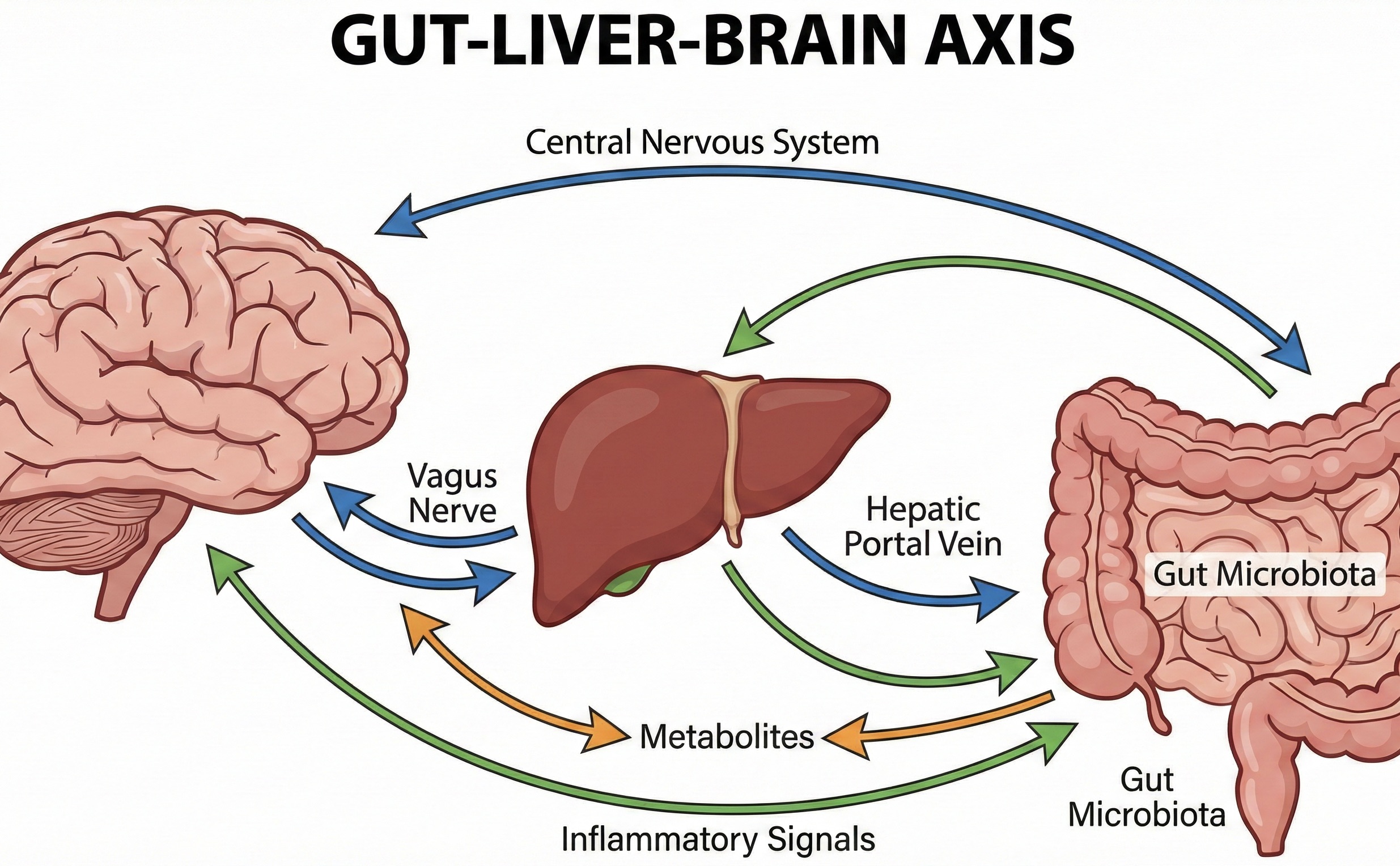
How It Works
The gut produces metabolites, neurotransmitters, and immune signals that travel to the liver and brain. A large proportion (often estimated around 70%) of the body’s immune cells reside in the gut‑associated lymphoid tissue, making the gut a major regulator of systemic inflammation.
When the intestinal barrier is intact, it allows nutrients through while blocking bacteria and toxins. When the barrier weakens (intestinal permeability or "leaky gut"), lipopolysaccharides (LPS) and other bacterial products enter the bloodstream and travel to the liver.
The liver responds by activating immune cells called Kupffer cells. These release inflammatory cytokines that:
- Elevate liver enzymes (ALT, AST, GGT).
- Increase oxidative stress.
- Promote fat accumulation in liver cells.
- Cross the blood-brain barrier and affect brain function.
This is why gut dysfunction often shows up as elevated liver enzymes and brain fog at the same time.
Not all disruptors are equal. Some affect the axis within days. Others build up over weeks or months
Acute disruptors (effects within days):
Alcohol - Damages the gut lining directly, kills beneficial bacteria, and allows endotoxins to flood the liver. Even a single heavy drinking episode can temporarily increase intestinal permeability.
Antibiotics - Disrupt gut bacteria balance rapidly. A single course can alter the microbiome for weeks to months.
Sleep deprivation - Alters gut bacteria composition within 48 hours and increases systemic inflammation.
Acute stress - Activates the vagus nerve and HPA axis, immediately affecting gut motility and barrier function.
Chronic disruptors (effects build over weeks/months):
Diet pattern - Processed foods, excess sugar, and low fiber feed harmful gut bacteria and weaken the intestinal barrier over time. High-fat, high-sugar diets can increase permeability within days, but the microbiome shift is gradual.
Ongoing stress - Chronic stress reduces beneficial gut bacteria populations and creates sustained low-grade inflammation.
Metabolic dysfunction - Insulin resistance and elevated blood sugar promote gut inflammation and alter the microbiome. This creates a cycle where gut dysfunction worsens metabolic health, which worsens gut dysfunction.
Certain medications - NSAIDs, proton pump inhibitors, and some other medications can weaken the gut barrier with prolonged use.
What This Looks Like on Lab Work
A common pattern suggesting gut-liver axis stress: GGT is elevated (say, 35-50 U/L in men, 20-30 U/L in women) while ALT stays normal or only mildly elevated.
This suggests oxidative stress from gut-derived endotoxins rather than direct liver cell damage. The liver is processing inflammatory signals from the gut, which elevates GGT, but the liver cells themselves aren't injured yet, so ALT stays relatively stable.
If ALT were the primary elevation with normal GGT, you'd look for other causes: medication effects, viral hepatitis, or intense recent exercise.
The AST:ALT ratio matters too. A ratio below 1 (ALT higher than AST) is typical in metabolic and gut-related liver stress. A ratio above 2 suggests alcohol-specific damage.
GGT is particularly sensitive to gut-liver axis dysfunction. It often elevates before ALT because it reflects oxidative stress from endotoxin exposure.
How to Support the Gut-Liver-Brain Axis
Supporting this system involves:
- Eating fermented foods (yogurt, kimchi, sauerkraut, kefir).
- Consuming prebiotic fiber (vegetables, legumes, whole grains).
- Limiting processed foods and added sugars.
- Managing stress through sleep, exercise, or mindfulness.
- Reducing or eliminating alcohol if enzymes are elevated.
- Getting 7-9 hours of sleep consistently.
The gut microbiome is resilient. Research shows beneficial changes in gut bacteria within days of dietary improvements.
The Alcohol Connection
Alcohol specifically damages the gut-liver-brain axis through multiple pathways. Research from NIAAA shows alcohol:
- Kills beneficial gut bacteria and increases harmful bacteria.
- Weakens the intestinal barrier directly.
- Allows bacterial endotoxins to flood the liver.
- Triggers oxidative stress that elevates GGT.
If you are doing Dry January or an alcohol break, testing GGT before and after shows exactly how your gut-liver axis responds.
Recovery Timeline
Remember: you may feel better before your labs normalize. This is normal and expected. When the underlying cause is addressed, the gut-liver-brain axis begins recovering quickly:
Days 1-7 - Gut bacteria begin rebalancing. Many people notice improved sleep, mood, and mental clarity here, even though liver enzymes haven't budged yet.
Weeks 2-4 - GGT typically shows measurable improvement. Systemic inflammation decreases. This is when labs start catching up to how you feel.
Weeks 4-8 - ALT and AST normalize in most cases. Gut barrier function largely restored.
Months 2-6 - Full gut microbiome rebalancing. Continued liver healing. Sustained improvements in energy and cognition.
The Takeaway
The gut-liver-brain axis explains a pattern many people experience: feeling mentally foggy and run down even when nothing seems "wrong." It also explains why some people feel sharper within days of changing their diet or cutting alcohol, while their liver enzymes take weeks to catch up.
Curious to undertsand where your liver stands? Explore our liver health survey below to get your liver's score in 5 minutes or less.









