Alcohol depletes B vitamins through multiple mechanisms. It reduces absorption, impairs storage, increases excretion, and interferes with conversion to active forms. For people recovering from regular alcohol use, B vitamin repletion is one of the most evidence-based interventions for supporting liver recovery.

According to research from the National Institute on Alcohol Abuse and Alcoholism, alcohol affects B vitamin status through several mechanisms:
Reduced absorption: Alcohol damages the intestinal lining and impairs the absorption of thiamine, folate, and B12 from food and supplements.
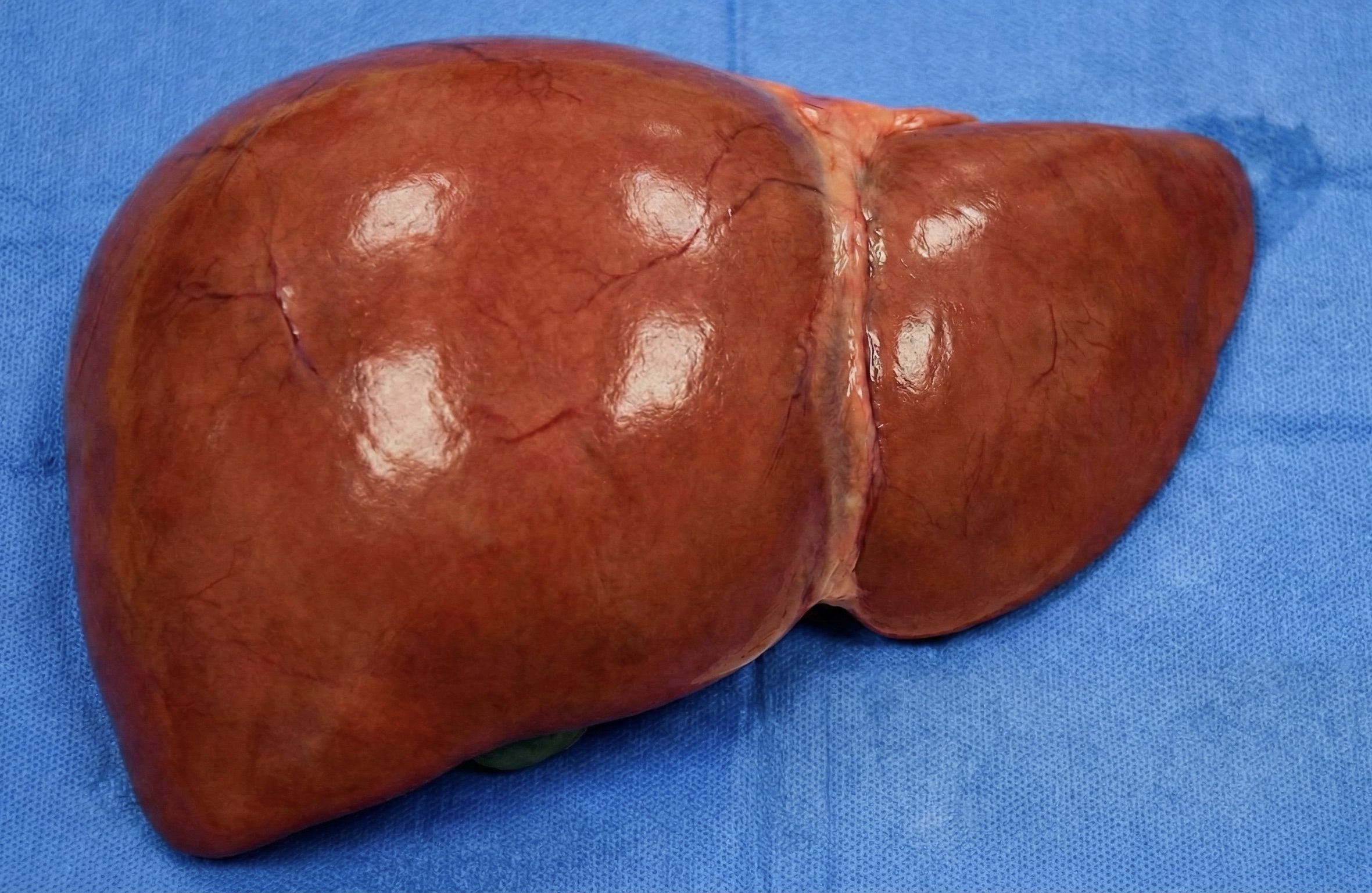
Impaired storage: The liver stores several B vitamins. Alcohol-related liver damage reduces the liver's capacity to store these nutrients.
Increased excretion: Alcohol has diuretic effects that increase urinary excretion of water-soluble B vitamins.
Blocked conversion: The liver converts B vitamins to their active forms. Alcohol interferes with these conversion processes.
These effects are cumulative. Regular drinking over months or years can produce significant B vitamin depletion even with adequate dietary intake.
Key B Vitamins for Liver Health
Thiamine (Vitamin B1):
Thiamine deficiency is one of the most serious nutritional consequences of heavy alcohol use. The liver requires thiamine for carbohydrate metabolism and energy production.
According to research in Alcohol and Alcoholism, up to 80 percent of people with alcohol use disorder have some degree of thiamine deficiency. Severe deficiency causes Wernicke-Korsakoff syndrome, a serious neurological condition.
The active form of thiamine is thiamine pyrophosphate (TPP). Some supplements provide thiamine in forms that may bypass absorption issues, including benfotiamine.
Folate (Vitamin B9):
Folate deficiency is common in people who drink regularly. Alcohol blocks folate absorption and interferes with folate metabolism in the liver.
Research published in the Journal of Nutrition found that alcohol consumption is associated with lower folate levels even when dietary intake is adequate. Folate is essential for DNA synthesis and liver cell regeneration.
The active form is methylfolate (5-MTHF). Supplements providing methylfolate bypass the conversion steps that alcohol impairs.
Vitamin B12:
B12 deficiency can develop with chronic alcohol use. The liver stores B12, and alcohol-related liver damage can reduce storage capacity.
Research in the European Journal of Clinical Nutrition found lower B12 levels in people with alcohol-related liver disease compared to controls. B12 works closely with folate in methylation pathways important for liver function.
The active forms are methylcobalamin and adenosylcobalamin. These bypass conversion steps required for cyanocobalamin, the form in many supplements. Often times magenisum can help support B12 optimization.
Vitamin B6:
B6 is involved in over 100 enzyme reactions, including many in the liver. Alcohol accelerates B6 degradation and reduces blood levels.
B6 deficiency can contribute to elevated homocysteine, an inflammatory marker associated with cardiovascular and liver disease. The active form is pyridoxal-5-phosphate (P5P).
Clinical Research on B Vitamin Supplementation
Thiamine supplementation:
Clinical guidelines recommend thiamine supplementation for all patients with alcohol use disorder. Hospital protocols typically use high-dose intravenous thiamine initially, followed by oral supplementation.
For oral supplementation in non-acute settings, doses of 100 to 300 mg daily are commonly used. Benfotiamine, a fat-soluble form, may have better bioavailability.
Folate and B12 supplementation:
Research on folate supplementation in people with alcohol-related liver disease shows improvements in folate status and potential benefits for liver regeneration.
A study in Hepatology found that adequate folate and B12 status was associated with better outcomes in patients with alcoholic liver disease.
B-complex supplementation:
Given that multiple B vitamins are affected by alcohol, B-complex supplementation addresses several deficiencies simultaneously. This approach is supported by clinical practice guidelines for alcohol recovery.
Dosing: What Clinical Practice Supports
B vitamin doses for liver repair after alcohol use are typically higher than standard RDA values.
Duration: B vitamin repletion typically requires consistent supplementation for 8 to 12 weeks. Longer durations may be needed for severe depletion.
Form considerations: Active (methylated) forms of B vitamins do not require liver conversion, which may be impaired in people with liver stress. Look for methylfolate, methylcobalamin, and pyridoxal-5-phosphate on labels.
B-Complex Products by Formulation Type
Standard B-Complex (basic forms):
Methylated B-Complex (active forms)
High-Potency Thiamine Products
Safety and Considerations
B vitamins are water-soluble, and excess amounts are generally excreted in urine. Toxicity is rare at supplemental doses.
Considerations:
- High-dose B6 (over 200 mg daily long-term) can cause nerve issues in some people. Standard B-complex doses are well below this threshold.
- High-dose folate can mask B12 deficiency symptoms. Supplementing both together avoids this issue.
- B vitamins may cause bright yellow urine. This is harmless and indicates excretion of excess riboflavin (B2).
According to the NIH Office of Dietary Supplements, B vitamins have wide safety margins at doses used for repletion.
How to Measure If B Vitamins Help Your Liver
B vitamin supplementation supports liver function indirectly by correcting deficiencies that impair liver cell metabolism and regeneration.
The objective approach is testing liver markers before starting supplementation and again after 8 to 12 weeks.
Key markers to track:
- ALT - reflects liver cell health (optimal: men below 55 U/L, women below 45 U/L)
- AST - reflects liver and muscle stress (optimal: men below 45 U/L, women below 35 U/L)
- GGT - reflects oxidative stress (optimal: men below 14 U/L, women below 9 U/L)
B vitamin supplementation alone may not dramatically change liver enzymes if other factors like ongoing alcohol use or metabolic issues are present. But correcting deficiencies supports the liver's overall capacity to recover.
For context on interpreting these markers, review the guide on liver function testing.
A Research-Based Approach
Based on clinical evidence:
- Alcohol depletes multiple B vitamins through several mechanisms
- Thiamine, folate, and B12 are most commonly affected
- Active (methylated) forms bypass impaired liver conversion
- Clinical repletion doses are higher than standard RDA values
- Testing liver markers provides objective data on liver recovery progress
B vitamin supplementation is one of the most evidence-supported interventions for people recovering from regular alcohol use. Testing helps you track whether your liver is responding to this and other changes you are making.
Learn how to establish baseline markers and track your progress with at-home liver function testing.
Track Your Recovery
B vitamin repletion is a foundational step for liver recovery after alcohol use. The research supports supplementation, particularly with active forms that do not require liver conversion.
But knowing whether your liver is actually recovering requires measurement. Testing before and after supplementation, combined with alcohol reduction and other lifestyle changes, shows you objective progress.
Test your liver's score with our liver health survey in 5 minutes below.

.png)