What You'll Learn:
- How insulin resistance causes fat buildup in the liver
- Why fatty liver makes insulin resistance worse
- Which markers reveal this metabolic connection
- How to track both liver and metabolic health together

How Insulin Resistance Affects Your Liver
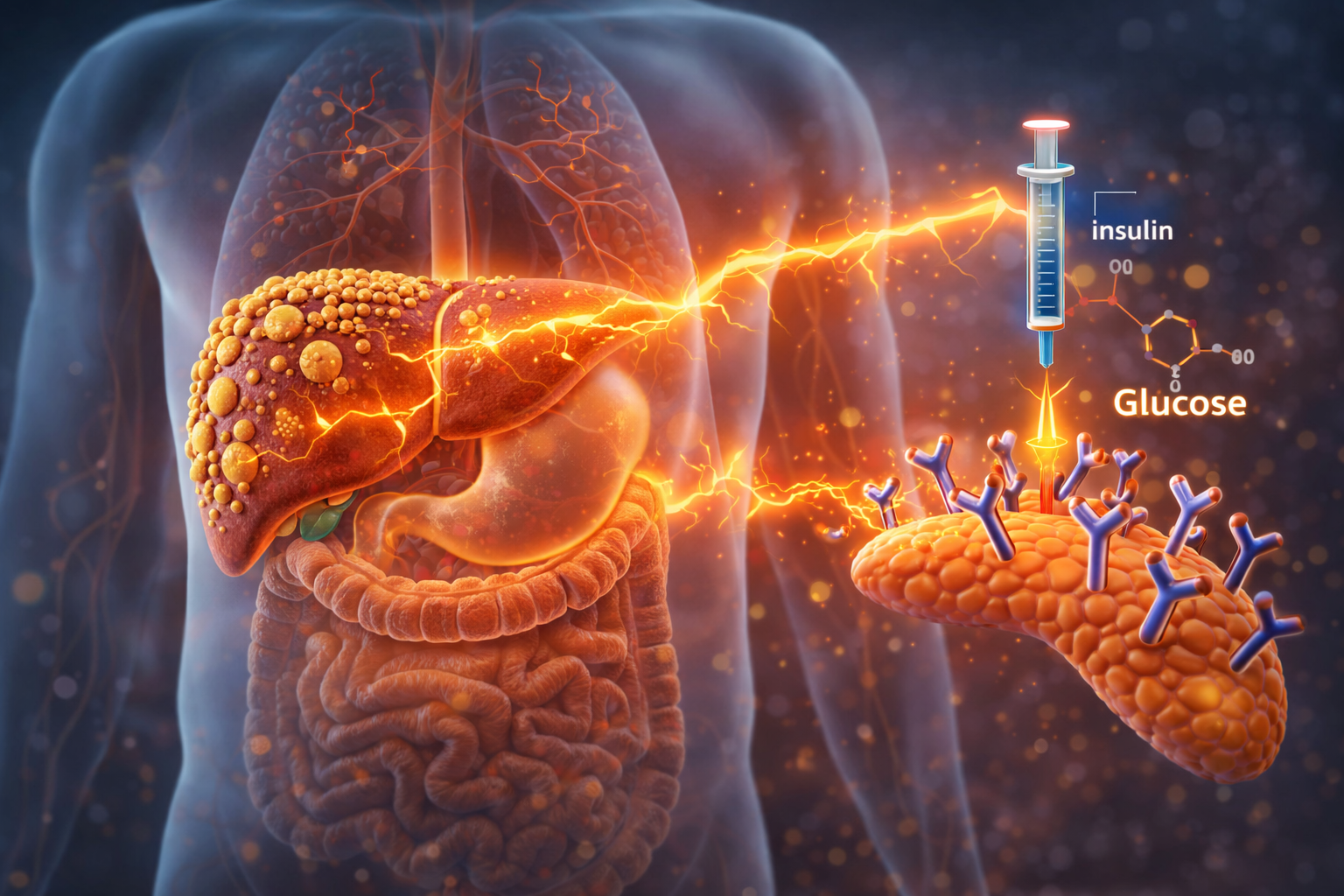
When your cells become resistant to insulin, your body compensates by producing more of it. High circulating insulin levels trigger a cascade of problems in the liver.
First, elevated insulin tells your liver to convert excess glucose into fat. This process, called de novo lipogenesis, increases dramatically in insulin-resistant states. The fat accumulates inside liver cells.
Second, insulin resistance impairs your liver's ability to burn fat for energy. Normally, the liver can switch between burning glucose and burning fat depending on what's available. Insulin resistance disrupts this flexibility.
Third, high insulin levels prevent the release of stored fat from adipose tissue. This sounds like it would reduce liver fat, but it actually backfires. The liver ends up synthesizing more fat internally because it can't access fat from other storage sites.
How Fatty Liver Makes Insulin Resistance Worse
The relationship works both directions. Once fat accumulates in liver cells, it actively promotes insulin resistance.
Research from Yale University found that hepatic fat content is the strongest predictor of insulin resistance in patients with fatty liver disease. Specifically, a type of fat molecule called diacylglycerol (DAG) accumulates in liver cells and interferes with insulin signaling.
This creates a vicious cycle:
- Insulin resistance increases liver fat
- Liver fat worsens insulin resistance
- Worsening insulin resistance increases liver fat further
- The cycle continues unless interrupted
Breaking this cycle requires addressing both problems simultaneously. Weight loss, exercise, and dietary changes can improve both liver fat and insulin sensitivity together. Detoxifying the liver via alcohol reduction is one of the best ways to ensure success.
The Numbers: Where These Problems Intersect
Studies show striking overlap between fatty liver and metabolic dysfunction:
The metabolic dysfunction driving fatty liver typically shows up in blood markers before symptoms appear. This is why testing matters, especially if you have risk factors like abdominal obesity, family history of diabetes, or elevated triglycerides.
Which Markers Reveal the Connection
Testing both liver enzymes and metabolic markers together gives you the complete picture. Here's what to track:
The combination of elevated GGT with borderline HbA1c strongly suggests the liver-insulin resistance connection is active in your body. Monitoring ALT aongside AST is the best way to understand these markers.
Why ALT and GGT Rise Before Blood Sugar
Here's something most people don't realize: liver enzymes often elevate years before blood sugar markers change. Research confirms that ALT and GGT predict future diabetes risk even when fasting glucose is still normal.
This happens because the liver is the first organ to experience metabolic stress from insulin resistance. By the time blood sugar rises enough to flag as prediabetic, the liver has usually been accumulating fat for years.
Testing liver enzymes alongside HbA1c and fasting glucose catches metabolic dysfunction earlier. Earlier detection means easier reversal.
Breaking the Cycle
The good news: this cycle can be broken. Weight loss of just 5-10% often produces significant improvements in both liver fat and insulin sensitivity.
What works:
- Reducing refined carbohydrates and added sugars
- Increasing physical activity (both cardio and resistance training)
- Prioritizing sleep (poor sleep worsens insulin resistance)
- Managing stress levels (cortisol impairs insulin sensitivity)
Most people see liver enzymes improve within 4-8 weeks of consistent lifestyle changes. Metabolic markers like HbA1c take longer, usually 2-3 months to reflect improvements.
Track Both Together
Because liver and metabolic health are so interconnected, tracking them together makes sense. Testing both sets of markers every 3-6 months helps you see whether your approach is working.
Many people feel better before their numbers fully normalize. That's encouraging, but the real goal is getting your markers into optimal ranges and keeping them there long-term.









